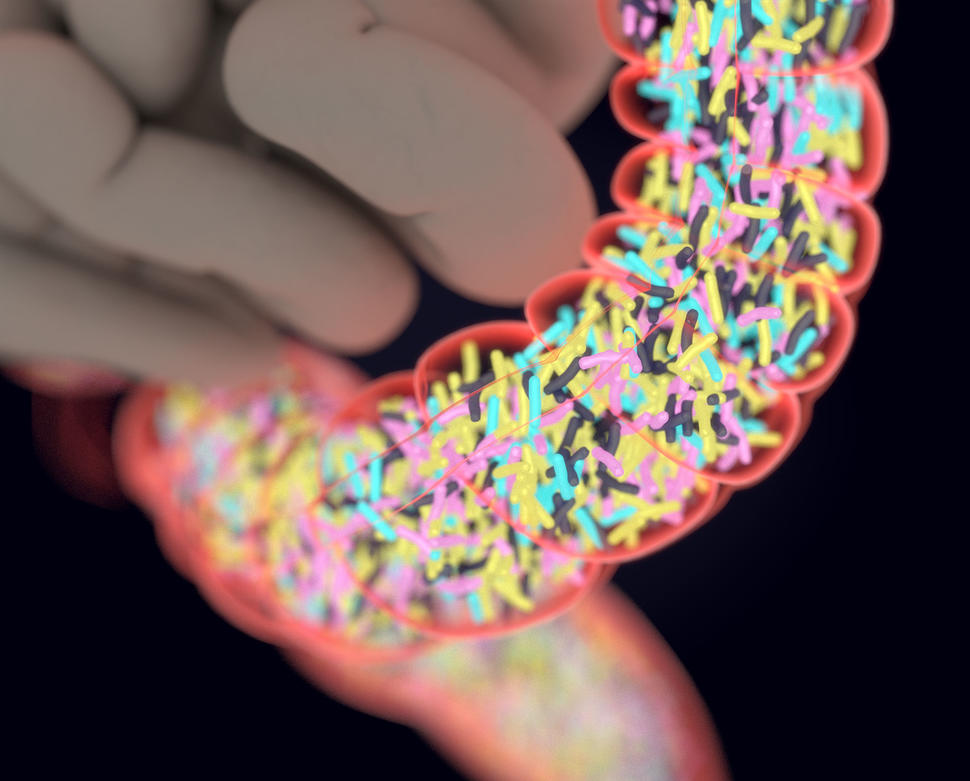
Earlier this month, the National Cancer Institute (NCI) of the National Institutes of Health (NIH) published a press release concerning the usage of fecal transplants to augment immunotherapy in advanced skin cancer patients. According to the NCI, patients with advanced melanoma responded more favorably to immunotherapy drugs after receiving a transplant of fecal microbiota from other drug responders.
“Our study is one of the first to demonstrate in patients that altering the composition of the gut microbiome can improve the response to immunotherapy,” said Giorgio Trinchieri, chief of the Laboratory of Integrative Cancer Immunology at the NCI. “The data provides proof of concept that the gut microbiome can be a therapeutic target in cancer.”
Gut bacteria has previously been shown to be an effective booster for certain forms of immunotherapy, with a 2018 study showing favorable results in treating mice with melanoma using human gut bacteria. According to the NCI, 6 out of 15 patients who had previously not responded to immunotherapeutic drugs experienced long-term disease stabilization and tumor reduction after the fecal transplants.
Cancer research has recently also emerged from the Korea Institute of Science and Technology (KIST) publishing two new research results last month. KIST’s Biomaterials Research Center reported on a newly-developed test for diagnosing prostate cancer in men using AI to examine urinary samples. The test is capable of diagnosing prostate cancer within twenty minutes of sample examination with nearly 100% accuracy between 76 cancer-positive samples.
The tool uses data-trained AI that detects common cancer signifiers in urine with ultrasensitive sensors capable of cross-examining symptoms and comparing them to results from previous prostate cancer patients.
The accuracy and efficiency of the treatment is much better than the 30% accuracy of the Prostate-Specific Antigen (PSA) blood test normally used for prostate cancer diagnosis. KIST’s urinary test is just one of many new cancer diagnosis methods that use AI analysis to improve diagnosis accuracy, with the NCI developing their own AI-driven tool to diagnose cervical cancer with exceeding results last year.
“This research developed a smart biosensor that can rapidly diagnose prostate cancer with almost 100 percent accuracy only through a urine test, and it can be further utilized in the precise diagnoses of other cancers using a urine test,” said Dr. Kwan Hyi Lee of KIST’s Biomaterials Research Center.
KIST’s other current research includes new phototherapy methods that use light to mitigate the pain and side effects induced by chemotherapy and decrease tumor remission. The treatment injects photosensitizers, which destroy cancer cells under exposure to light, into patients, who then undergo directed laser therapy to gradually reduce and eliminate tumors.
Because the phototherapy only affects the targeted area that contains the tumor, it does not damage nearby tissue in the caustic manner that is exhibited by chemotherapy or radiation therapy. This allows for more repeated, consistent and effective administration of treatment due to the lack of health concerns induced by the phototherapy.
The Theragnosis Research Center at KIST developed a new form of photosensitizer based on peptides that last in the body for two to four weeks, negating the need for repeated injections during each round of phototherapy. The phototherapy was tested on mice that experienced complete tumor reduction and recovery with no damage to surrounding tissues by the tumor.
The motherlode of treatment breakthroughs came earlier this month, too, with California-based biopharmaceutical company Amgen submitting a new drug for FDA approval, designed to inhibit specific gene mutations. The drug, Sotorasib, inhibits the mutation known as KRAS G12C, a gene mutation uncommonly found in non-small cell lung cancer (NSCLC) patients, as well as patients with diseases such as pancreatic and colorectal cancer. Sotorasib caused significant tumor reduction in all NSCLC patients that had the mutation, with three of the 126 patients experiencing complete cancer recovery.
Although NSCLC is one of the less lethal forms of cancer, other KRAS-adjacent cancers can be far more lethal, with pancreatic cancer exhibiting a 3% five-year survival rate for late-stage patients. New drugs and treatment methods like Sotorasib have the potential to reshape the way that society and the medical field approach treating and coping with cancer.